Poor Sleep
Created on August 5, 2017. Last updated on March 6th, 2024 at 04:50 pm
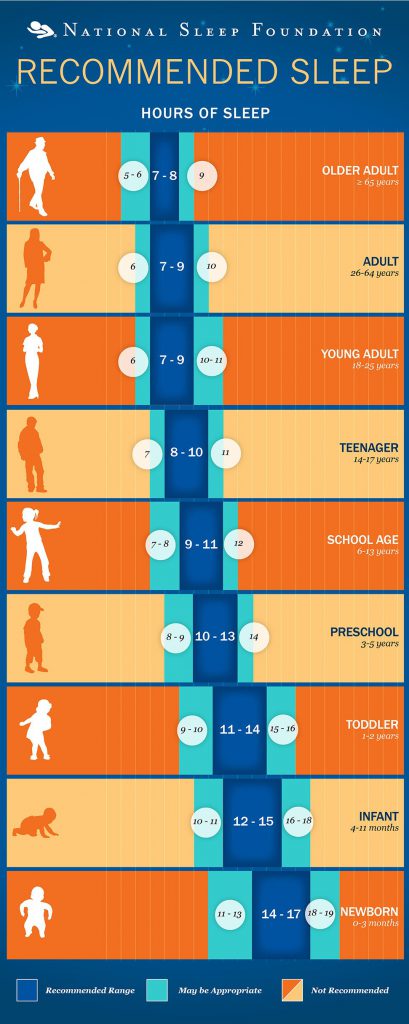
According to the National Sleep Foundation the amount of sleep we need depends a lot on our age. Infants should be getting between 14 and 17 hours of sleep per night, whereas teenagers should be getting between 8 and 10 hours per night. Not getting enough sleep impacts the way we think, our ability to focus, and our overall mood. Even if we go to bed at the right time, there’s still a chance that we may not be getting enough sleep. Many people have trouble falling asleep, staying, asleep, or just getting restful sleep. Sometimes this is due to a specific sleep disorder.
Pediatric Sleep Disorders:
- Sleep-Related Breathing Disorders (e.g., Obstructive Sleep Apnea)
- Sleep-Related Movement Disorders (e.g., Restless Leg Syndrome)
- Insomnia
- Parasomnias
- Circadian Rhythm Sleep Disorders
Other times poor sleep may be a side effect of something else happening in our lives. Sometimes it can be due to a specific situation (e.g., stress over a test coming up or excitement about going on a trip), but sometimes it can be due to a psychological disorder such as:
- ADHD
- Anxiety
- Depression
- Bipolar
- PTSD
Whether poor sleep is due to a sleep disorder or is a side effect of something else, it is important to seek treatment. Research has examined several effective approaches to treat sleep concerns.
While medication is commonly used to treat a variety of sleep concerns, there is limited data regarding dosing, effectiveness, tolerance, and safety of these medications, especially in children. Generally, cognitive behavioral/behavioral interventions are recommended as the first line treatment for sleep concerns in children.
| Level One: Works Well |
|
| Level Two: Works |
|
| Level Three: Might Work |
|
| Level Four: Unknown/Untested |
|
| Level Five: Tested and Does Not Work |
|
References:
Carney, Colleen & Edinger, Jack. (2010). Cognitive Behavior Therapy for Insomnia: Treatment Considerations Insomnia and Anxiety, 51-61. doi:10.1007/978-1-4419-1434-7_4
Changani, Bantu, Greydanus, Donald E., Patel, Dilip R. & Feucht, Cynthia. (2011). Pharmacology of Sleep Disorders in Children and Adolescents Pediatric Clinics of North America, 58(1), 273-291. doi:10.1016/j.pcl.2010.11.003
Haynes,J, Talbert,M, Fox,S & Close,E. (2018). Cognitive Behavioral Therapy in the Treatment of Insomnia. Southern medical journal, 111(2), 75-80. doi:10.14423/SMJ.0000000000000769
Hirshkowitz, M., Whiton, K., Albert, S. M., Alessi, C., Bruni, O., DonCarlos, L., … & Neubauer, D. N. (2015). National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health, 1(1), 40-43.
Means,MK, Lineberger,MD & Edinger,JD. (2008). Nonpharmacologic treatment of insomnia. Current treatment options in neurology, 10(5), 342-9.
Moturi, S., & Avis, K. (2010). Assessment and treatment of common pediatric sleep disorders. Psychiatry (Edgmont), 7(6), 24.
Useful Graphics